Abstract
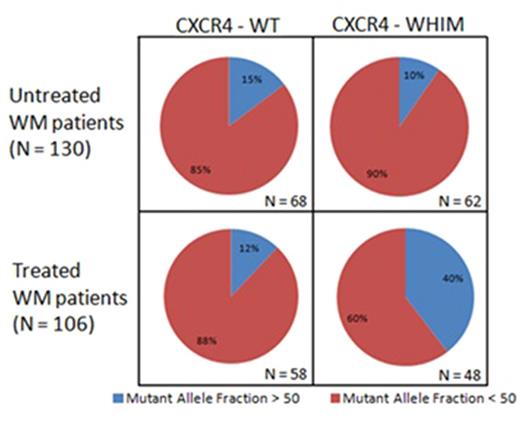
Somatic mutations affecting MYD88 are present in >90% of Waldenstrom's Macroglobulinemia (WM) patients, with nearly all of them being heterozygous [mutant allele frequency (MAF) <50%) and resulting from a change of leucine to proline at amino acid position 265. Previous studies in small study sets have observed that increased MYD88 homozygosity, i.e. MAFs >50% were present in 10-12% of untreated WM patients, a phenomenon that was attributed to acquired uniparental disomy (aUPD) and copy number alterations (Treon et al, NEJM 2012; Poulain et al, Blood 2013) at chromosome 3p. CXCR4 WHIM-like mutations are the second most common mutations in WM, affecting 30-40% of patients and almost always are associated with mutated MYD88 (Hunter et al, Blood 2014). Further to these studies, we evaluated the MAF of MYD88 in 236 WM patients (130 untreated and 106 previously treated), and observed MAFs >50% in 42/236 WM patients (17.8%), that was particularly striking in previously treated (26/106, 24.5%) versus untreated (16/130, 12.3%) patients (p = 0.017). To better understand the mechanism for increased MYD88 MAFs in WM, Sanger sequencing, copy number (CNA), and aUPD analysis were performed using CD19-selected BM mononuclear cells. Sanger sequencing of MYD88 L265P was used to establish the ratio of mutant versus wild-type allele expression. TaqMan real-time PCR assay was used to determine the MYD88 copy number. In total, 42 patients were screened for MYD88 copy number, with 6 patients (14.3%) being copy number altered (3 amplifications, 3 deletions).
For patients with a MAF >50%, and an unaltered copy number, the presence of aUPD was determined by analyzing the tumor/germline allele balance in as many as 14 germline heterozygous single nucleotide polymorphisms using TaqMan genotyping assays. Fifteen out of twenty-one (5 untreated, 10 previously treated) patients tested were determined to have aUPDs. Several of these patients were also validated using next-generation sequencing, with the percentage of MYD88 mutant reads highly correlating with our Sanger estimates (r=0.9). As shown in Figure 1, CXCR4 mutations were similarly distributed between untreated patients with a MYD88 MAF >50% (6/16, 37.5%) and MAF <50% (56/114, 49%). Patients with MYD88 MAF >50% did not differ significantly based on previous treatment status (p=0.063), except in the context of CXCR4. Among previously treated patients, CXCR4 mutations were more prevalent among those with a MYD88 MAF >50% (19/26, 73%) versus MAF <50% (29/80, 36%; p=0.001) (Figure 1). Nine out of 10 (90%) previously treated patients with aUPDs were also CXCR4-mutated versus 29/80 (36%) patients with a MYD88 MAF <50% who were CXCR4-mutated (p=0.0015). Only 1/5 (20%) untreated patients were CXCR4-mutated (p= 0.017 versus previously treated patients with aUPDs). Interestingly, more patients who had been treated with the BTK inhibitor ibrutinib had an MAF >50% (7/15, 46.7%) versus patients not treated with ibrutinib (19/91, 21%; p=0.049). Our findings show that mutated MYD88 homozygosity is increased in previously treated patients with Waldenstrom's Macroglobulinemia, and associates with CXCR4 mutation status and ibrutinib exposure.
Castillo: Abbvie: Research Funding; Janssen: Consultancy, Research Funding; Pharmacyclics: Consultancy, Research Funding; Millennium: Research Funding. Treon: Pharmacyclics: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal